Everything you need to prepare your mind, body, and life for pregnancy
During the first 60 days, many factors can affect fetal development, making preconception planning an essential first step for a healthy pregnancy. We highly recommend that you see your physician. They will review your health, family history, environment, and lifestyle to check for any inherited diseases and look for ways to help prevent complications and reduce the risk of birth defects—all to ensure the safety of your future baby.
Tips on How to Prepare For Pregnancy
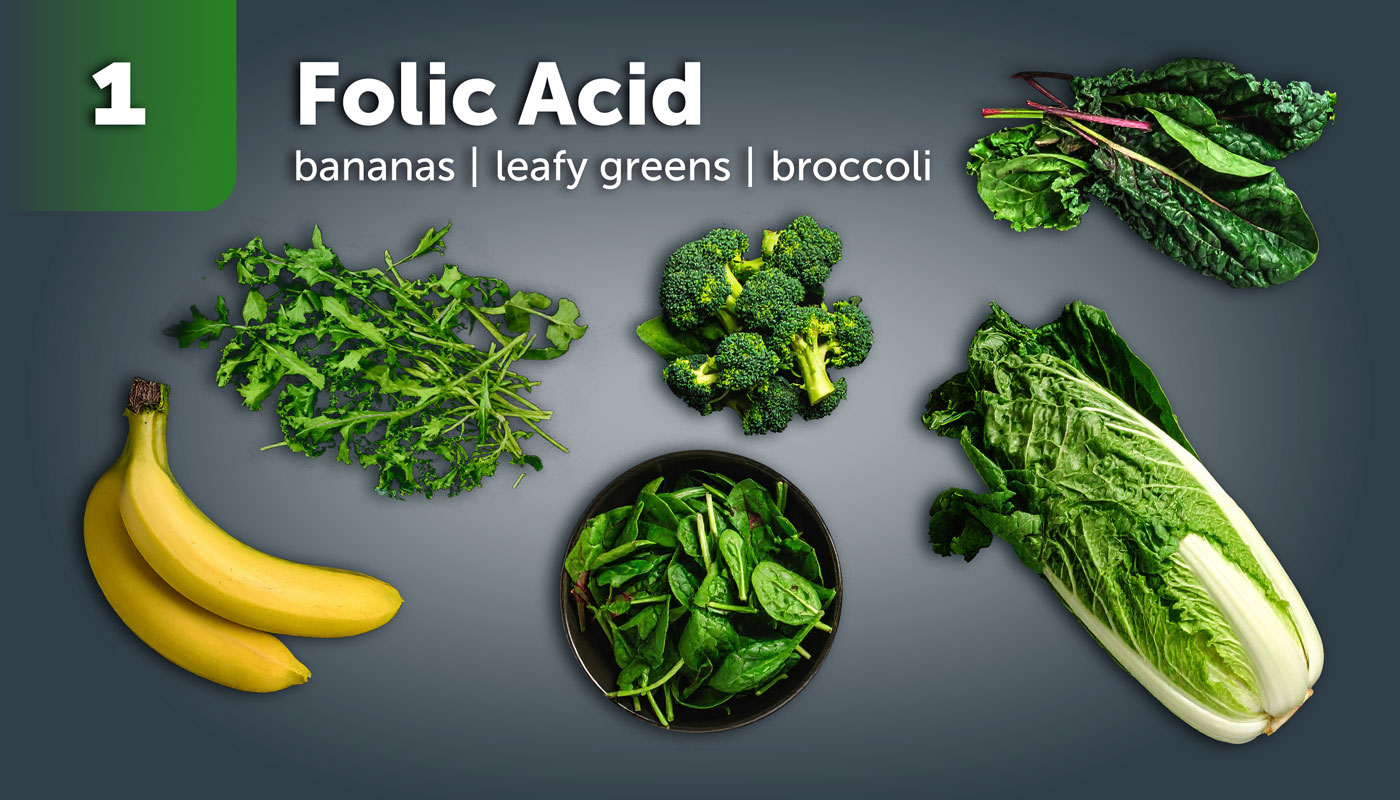
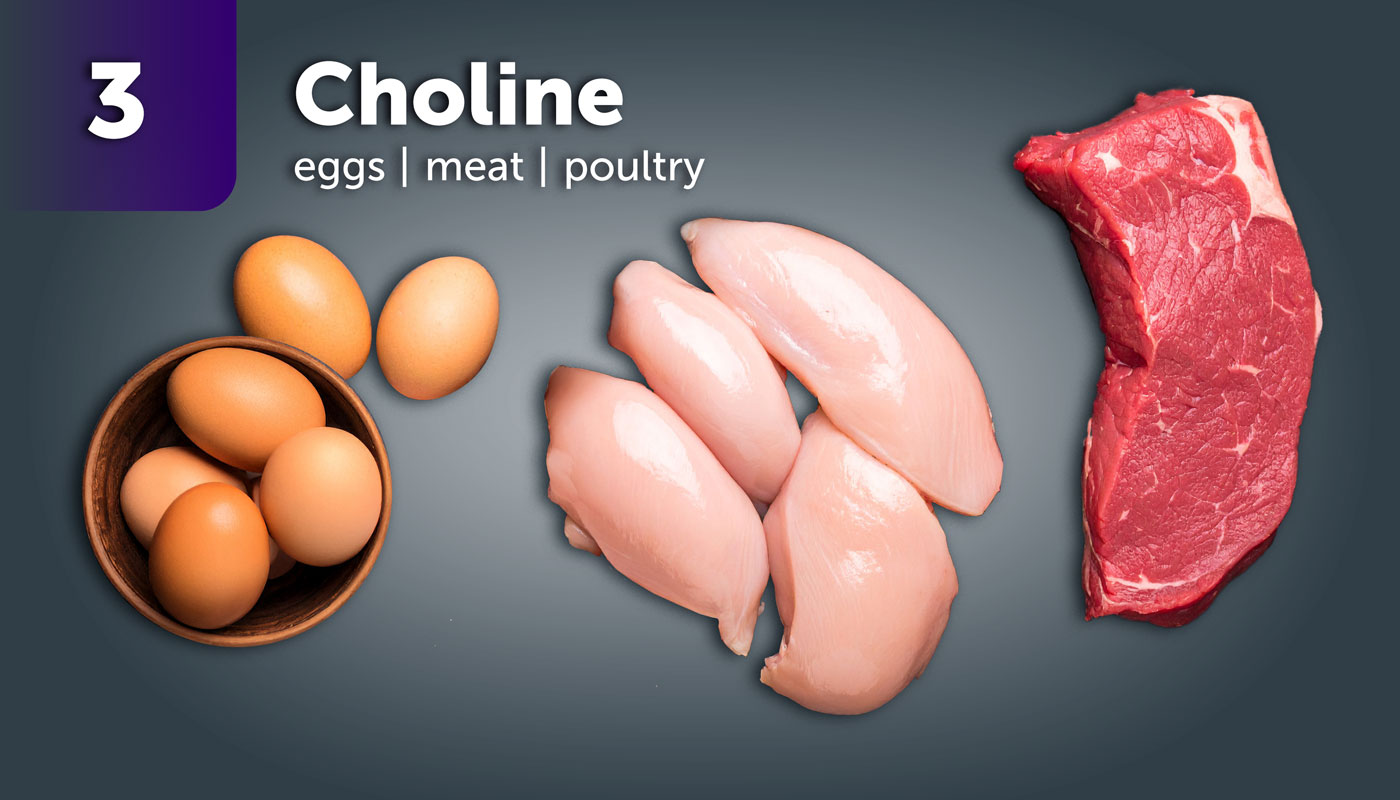
Top 5 Nutrients for a Healthy Pregnancy
Exercise, Sleep, and Healthy Weight Management
Regular physical activity can help regulate hormones, improve mood, reduce stress and prepare your body for the physical demands of pregnancy and childbirth. Talk to your OB or midwife before starting a new routine, especially if you have underlying health conditions.
- Goals for Exercise
- Aim for 150 minutes of moderate-intensity activity per week (e.g., brisk walking, swimming, biking)
- Include strength training 2 – 3 times per week
- Focus on low-impact activities that promote cardiovascular health and flexibility
- Tips for Exercise
- If you’re new to exercise, start with 10 – 15 minutes a day and build gradually
- Avoid high-risk sports or intense training without medical guidance
- Consider yoga or Pilates for core strength and stress relief
Sleep plays a vital role in hormonal regulation, immune function, and reproductive health. Poor sleep may impact menstrual cycles and ovulation.
- Goals for Sleep Health
- Aim for 7 – 9 hours of quality sleep per night
- Maintain a consistent bedtime and wake-up time
- Create a calming bedtime routine (limit screens, caffeine, and late meals)
- Tips for Sleep Health
- Try journaling, meditation apps, or progressive muscle relaxation before bed if you’re struggling with sleep
- If snoring, fatigue, or insomnia are ongoing, consider a sleep evaluation
Reaching and maintaining a healthy weight can improve fertility, reduce risks during pregnancy, and support a smoother recovery postpartum
- Guidance for Healthy Weight Management
- A healthy body mass index (BMI) range for conception is typically between 18.5 – 24.9, but every body is different
- Losing just 5 – 10% of body weight (if overweight) can improve ovulation and hormonal balance
- Gaining a healthy weight (if underweight) can also improve fertility outcomes
- Tips for Healthy Weight Management
- Focus on whole foods, balanced meals, and steady activity rather than rapid weight loss
- Work with a provider or dietitian to set personalized, realistic goals
- There is no such thing as “perfect”. Small, consistent steps make a big impact.
Why Quitting Smoking Matters:
- Even before conception, smoking can:
- Affect hormone levels and ovulation
- Increase the time it takes to get pregnant
- Reduce egg and sperm quality
- Increase the risk of miscarriage and ectopic pregnancy
- During pregnancy, smoking is linked to:
- Premature birth
- Low birth weight
- Sudden Infant Death Syndrome (SIDS)
- Tips to Quit Smoking
- Set a quit date and share it with your partner or support person
- Identify your smoking triggers and plan alternatives
- Replace smoking breaks with short walks, journaling, or deep breathing
Quit nicotine today by attending our smoking cessation classes.
Why It’s Best to Stop Alcohol Now:
- Alcohol can:
- Disrupt your menstrual cycle and hormone balance
- Affects ovulation and egg quality
- Make it harder to track your cycle accurately
- Increase the risk of birth defects, often before you even know you’re pregnant
- Tips to Quit Alcohol
- Switch to non-alcoholic alternatives like sparkling water with lime or mocktails
- Let friends and family know you’re cutting back for health reasons
- Skip social triggers like bars or late-night events while you build new habits
- If cutting alcohol feels difficult, talk to your provider. There’s no shame in needing help.
Schedule a Preconception Planning Appointment
Managing Chronic Conditions
Chronic conditions like diabetes, high blood pressure, thyroid disease, asthma and autoimmune disorders can affect fertility, pregnancy outcomes, and your baby’s development. Managing them early improves your chances for a healthier pregnancy and smoother postpartum recovery.
- Schedule a checkup to talk with your provider about your condition and pregnancy goals
- Review your medications with your provider to determine safety during pregnancy or if dosage changes are needed
- For conditions like diabetes or hypertension, monitor your numbers regularly and aim for pregnancy-safe ranges
- Healthy eating, movement, stress management, and sleep are all tools to help manage your condition and prep your body for pregnancy
- You may need a collaborative plan with specialists (endocrinologist, cardiologist, maternal-fetal-medicine specialist) to support your journey
Fertility and Timing
Ovulation is when your ovary releases a mature egg, typically 12 – 16 days before your next period. This is your fertile window, when you’re most likely to conceive.
- An average woman’s fertile window lasts five – six days. Sperm can live in your body for up to five days.
- Your best chance of pregnancy occurs when you have intercourse one – two days before ovulation.
- A small rise in basal body temperature indicates that ovulation has occurred.
- Consider tracking ovulation for two – three months before trying to conceive to understand your body’s ovulation cycle and pattern.
- Conditions like PCOS, thyroid disorders, or stress can affect ovulation.
Ovulation Predictor Kits (OPKs) are an easy way to track ovulation. They are an at-home urine test that detects a surge in luteinizing hormone (LH), signaling that ovulation is likely to happen within the next 24 – 36 hours. OPKs are available at most drugstores.
There’s a lot of advice out there about getting pregnant, but not all of it is true.
Myth #1: If you’re healthy, you’ll get pregnant right away
Even healthy couples can take time to conceive. On average, it takes 6 – 12 months for many couples trying naturally. Age, timing, and other factors all play a role.
Myth #2: You can get pregnant any time during your cycle
You can only get pregnant during your fertile window, which is about 5 – 6 days before ovulation. Tracking ovulation helps identify your most fertile days.
Myth #3: Men’s fertility doesn’t decline with age
While men can remain fertile longer than women, sperm quality declines with age, and older paternal age has been linked to certain risks for baby.
Myth #4: You don’t need to see a doctor until after a year of trying
If you’re under 35 and have been trying for 12 months, or over 35 and trying for 6 months, it’s time to talk to a provider. You should also seek help earlier if you have irregular periods, a known condition (like PCOS or endometriosis), or concerns about sperm health.
Myth #5: Birth control delays fertility for months or years
For most people, fertility returns quickly after stopping birth control. Some methods (like the Depo shot) may take longer, but many can conceive within weeks or months.
Myth #6: Stress causes infertility
Stress alone doesn’t cause infertility, but chronic stress may interfere with ovulation or sexual desire. Managing stress is good for your overall health, but fertility issues usually have a medical cause.
Myth #7: You don’t need to worry about fertility until your 40s
Fertility starts to decline in your early 30s and more noticeably after 35. It’s still very possible to get pregnant, but understanding your fertility timeline can help you plan ahead.
Myth #8: Position, timing, or supplement can guarantee pregnancy
No single tip or trick guarantees conception. A healthy lifestyle and understanding your cycle help, but sometimes medical guidance is needed.
Fertility and Age
When to Seek Fertility Evaluation
It's important to understand how age impacts fertility and what you can do to plan ahead.
Mental and Emotional Preparation
Why Mental Health Matters in Preconception
Stress and emotional strain can affect:
- Hormonal balance and menstrual regularity
- Sleep quality, energy, and decision-making
- Relationship dynamics and communication
- Coping during pregnancy and postpartum
Untreated anxiety, depression, or trauma can also increase the risk of complications during and after pregnancy, including postpartum depression.
Tips for Managing Stress and Building Emotional Readiness

Create Mental Space
- Prioritize rest and self-care
- Set boundaries with stressful people or environments
- Practice saying "no" without guilt

Build a Mind-Body Routine
- Try mindfulness apps, yoga, or guided meditation
- Incorporate walks, stretching or movement into your day
- Keep a gratitude or reflection journal

Talk it Out
- Schedule time with a trusted friend, partner, or therapist
- Consider short-term counseling to explore fears or uncertainty
- Ask your provider for a referal to a behavioral health specialist if needed

Know Your History
- If you've had mental health conditions in the past, make a plan with your provider
- Some medications may need to be adjusted or discontinued during pregnancy. Don't stop without support.